Environmental Determinants of Amyotrophic Lateral Sclerosis (ALS): Pathways, Mechanisms, and Emerging Challenges
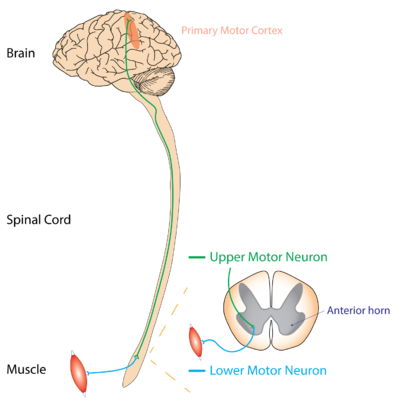
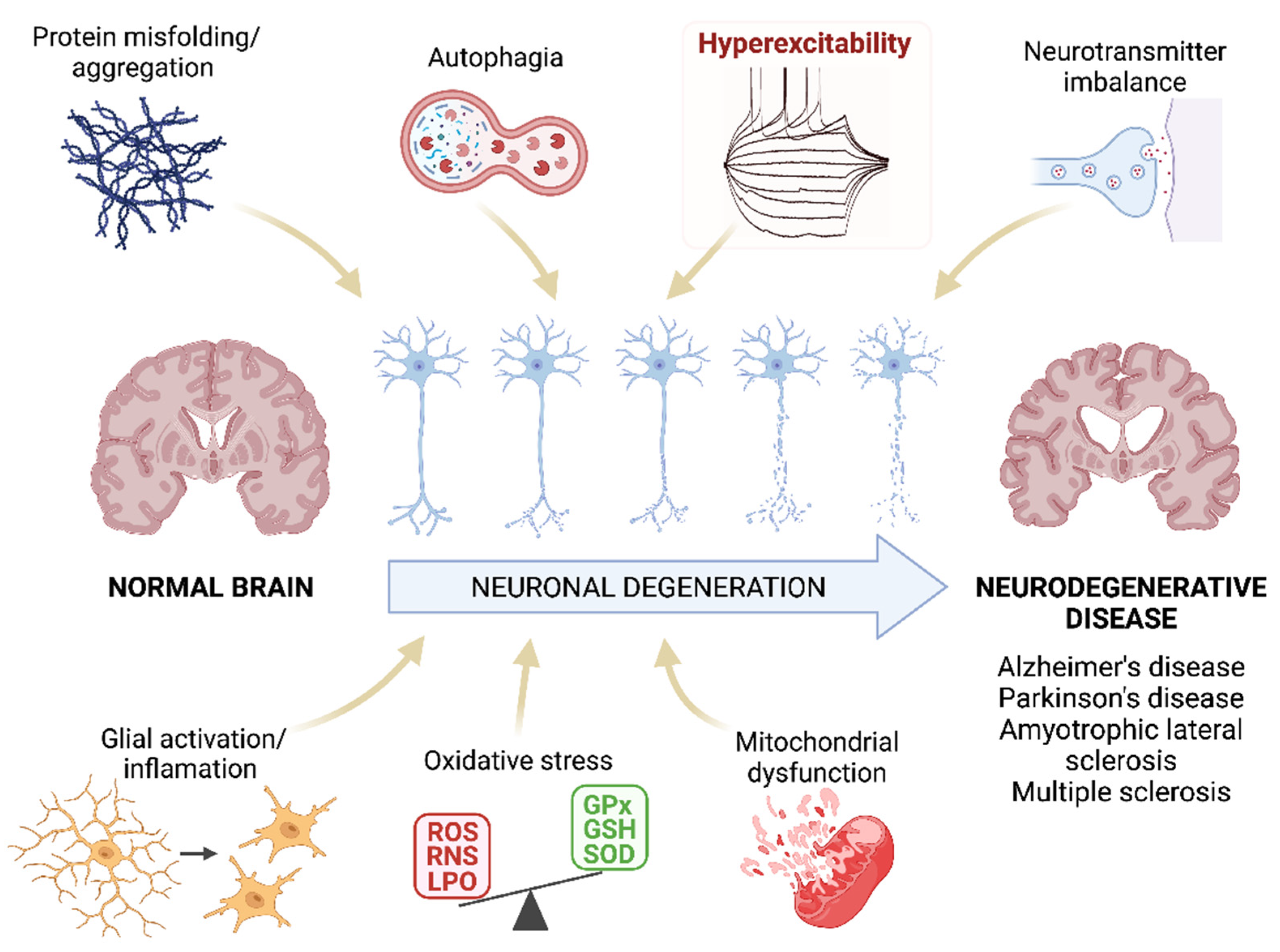
Amyotrophic lateral sclerosis (ALS) is a progressive and fatal neurodegenerative disorder characterized by the degeneration of upper and lower motor neurons. Clinically, it leads to muscle weakness, paralysis, and eventual respiratory failure. Traditionally, ALS has been framed largely as a neurological or genetic disease. However, this perspective fails to fully explain the epidemiology of the disorder.
Approximately 90–95% of ALS cases are sporadic, occurring without a clear familial or inherited genetic background. The predominance of sporadic ALS has shifted scientific attention toward environmental, occupational, and geographic determinants that may initiate or accelerate neurodegenerative processes. Increasingly, ALS is understood as a multifactorial disease, emerging from long-term interactions between environmental exposures and individual biological susceptibility.

Epidemiology and Spatial Patterns
ALS incidence varies markedly across regions, occupations, and environmental contexts. While the disease is globally rare, its non-random geographic distribution suggests that place-based exposures play a significant role.
Geographic clustering
Clusters of elevated ALS incidence have been reported in:
Industrial and mining regions
Intensive agricultural zones
Areas with documented air, soil, or water contamination
These clusters often persist across generations despite population turnover, indicating that environmental conditions rather than shared genetics may drive localized risk.
Occupational exposure patterns
Occupational groups repeatedly shown to have higher ALS risk include:
Farmers and pesticide applicators
Industrial and manufacturing workers
Construction workers
Military personnel
These occupations share chronic exposure to chemical toxicants, metals, solvents, and physical stress, strengthening the link between workplace environment and neurodegeneration.
Chemical and Toxic Environmental Exposures

Pesticides and herbicides
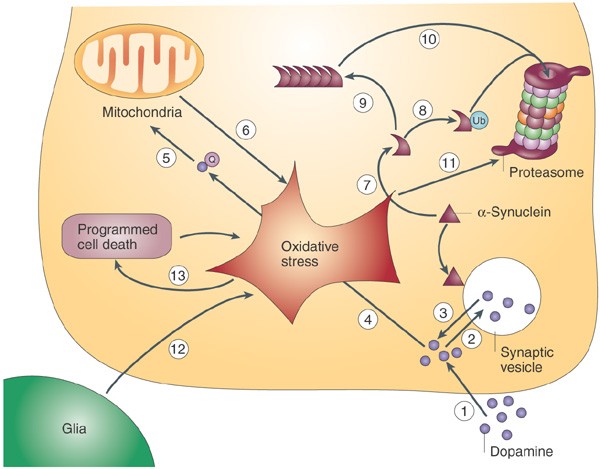
Among environmental risk factors, pesticide exposure has the strongest and most consistent association with ALS. Organophosphates, carbamates, and chlorinated pesticides are known to:
Disrupt neurotransmission
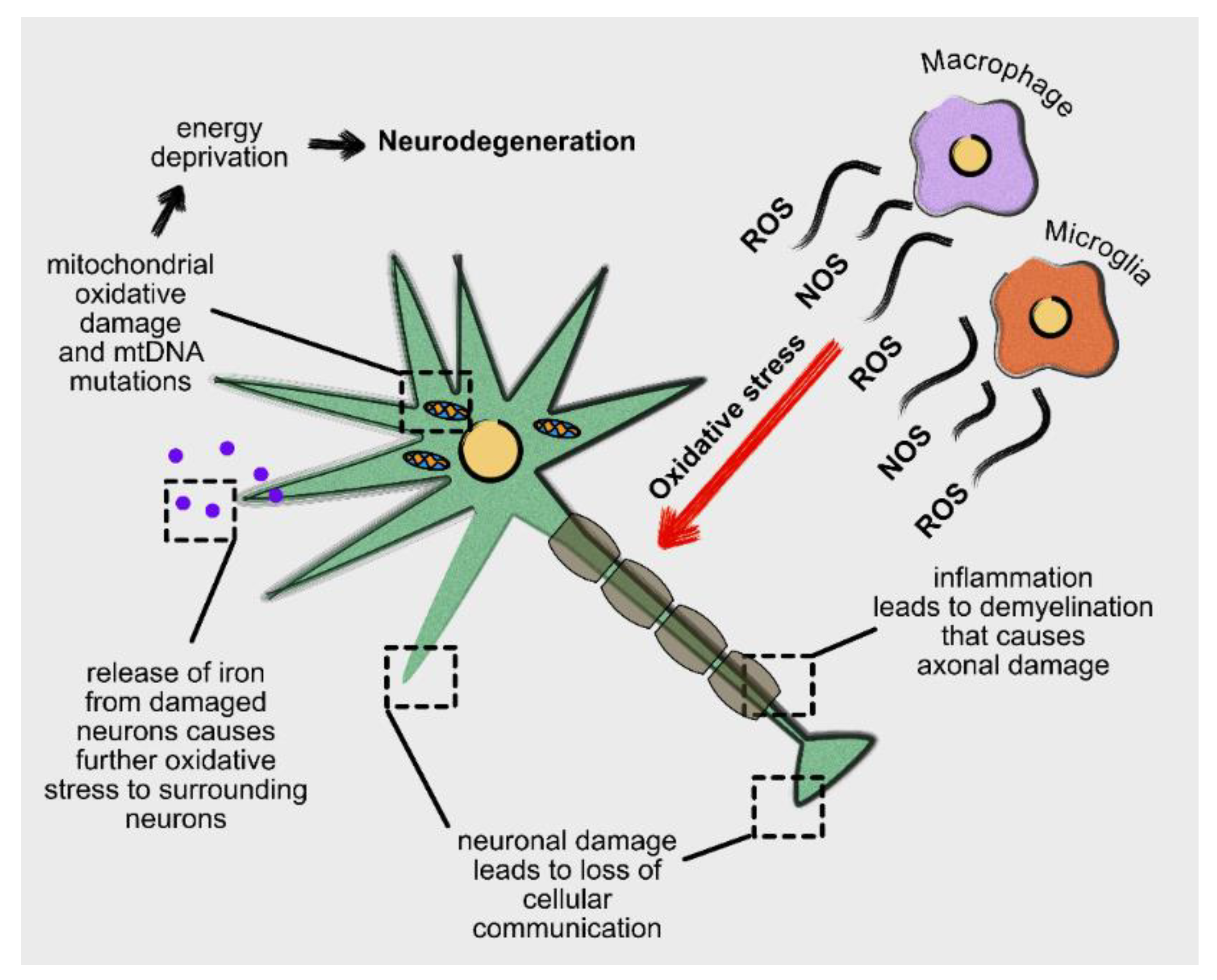
Induce oxidative stress
Damage mitochondrial function
Promote chronic neuroinflammation
Long-term, low-dose exposure—common in agricultural communities—may gradually overwhelm neuronal defense mechanisms, increasing vulnerability to degeneration.
Heavy metals
Heavy metals such as lead, mercury, cadmium, and arsenic accumulate in neural tissue and exert neurotoxic effects through:
Generation of reactive oxygen species
Disruption of calcium signaling
Impairment of DNA repair mechanisms
Elevated ALS prevalence has been observed near mining areas, battery manufacturing sites, and regions with industrial waste contamination.
Industrial solvents
Chronic exposure to solvents including formaldehyde, toluene, and trichloroethylene has been linked to motor neuron damage. These chemicals readily cross the blood–brain barrier and contribute to lipid membrane disruption and persistent inflammation.
Air Pollution and Neuroinflammation
Air pollution, particularly fine particulate matter (PM₂.₅), is increasingly implicated in neurodegenerative disease. Inhaled particles can:
Enter systemic circulation
Cross the blood–brain barrier
Activate microglial cells
Intensify oxidative stress
Long-term exposure to urban and industrial air pollution has been associated with earlier ALS onset and more rapid disease progression, highlighting air quality as a neurological as well as respiratory concern.
Cyanobacteria, Water Quality, and Neurotoxins
Cyanobacteria (blue-green algae) represent a unique environmental risk through the production of β-methylamino-L-alanine (BMAA), a neurotoxin linked to motor neuron degeneration.
BMAA:
Accumulates in freshwater and marine ecosystems
Enters food chains via fish, shellfish, and crops
Can be misincorporated into neuronal proteins
Regions experiencing frequent algal blooms have reported elevated ALS incidence, underscoring the role of water quality, eutrophication, and ecosystem disruption in neurological health.
Physical Stress, Trauma, and Occupational Load
Environmental risk does not operate solely through chemical exposure. Physical stressors may increase neuronal vulnerability, particularly when combined with toxic environments.
Factors associated with increased ALS risk include:
Repeated head injuries
Intense physical exertion
Military combat exposure
These stressors may accelerate neurodegeneration by increasing metabolic demand and inflammatory responses in already stressed neural systems.
Gene–Environment Interactions
Environmental exposures alone do not explain all ALS cases. Increasing evidence supports a gene–environment interaction model, in which environmental stressors activate latent biological vulnerabilities.
Environmental agents may:
Alter gene expression through epigenetic modification
Impair cellular stress-response pathways
Accelerate neuronal aging
This framework explains why ALS often appears later in life and why individuals with similar exposures experience different disease outcomes.
Lifestyle–Environment Overlap
Lifestyle factors do not independently cause ALS but may modify environmental risk.
Smoking
Smoking introduces heavy metals and oxidative agents that may amplify the neurotoxic effects of environmental exposures.
Dietary pathways
Contaminated food represents a significant exposure route:
Pesticide residues on crops
Heavy metals in fish and seafood
Algal toxins bioaccumulated through aquatic food chains
Chronic dietary exposure results in low-dose neurotoxicity that accumulates over decades.
Alcohol
Alcohol may function as a disease modifier by impairing detoxification pathways and increasing oxidative stress, rather than acting as a direct cause.
Soil and Groundwater Contamination
Soil and groundwater act as long-term reservoirs of environmental toxicants, particularly in rural and agricultural regions.
Persistent pesticides remain in soil for decades
Crops absorb metals and chemical residues
Groundwater contamination with arsenic and industrial effluents exposes entire communities
Chronic ingestion of contaminated water is a plausible but underexplored contributor to long-term neurodegenerative risk.
Climate Change as an Indirect Risk Amplifier
Climate change does not directly cause ALS, but it intensifies environmental exposure pathways.
Rising temperatures promote harmful algal blooms
Heat increases chemical toxicity and absorption
Shifting agricultural practices alter exposure profiles
Climate-driven ecological changes may therefore expand populations at risk and complicate disease prevention strategies.
Limitations and Scientific Uncertainty
Despite strong associative evidence, several challenges remain:
Long disease latency complicates exposure assessment
Reliance on self-reported exposure histories
Difficulty isolating individual toxicants from complex mixtures
Most findings remain associative rather than causal, and ALS heterogeneity further complicates risk modeling. Acknowledging these limitations strengthens scientific rigor and highlights the need for integrated, multidisciplinary research.
Amyotrophic lateral sclerosis is best understood not as a purely genetic or neurological disorder, but as the outcome of lifelong environmental interactions with vulnerable biological systems. Chemical pollutants, air and water contamination, occupational stress, lifestyle modifiers, and climate-driven ecological changes collectively shape ALS risk.
Viewing ALS through an environmental lens reframes it as a place-based public health challenge, demanding responses that extend beyond clinical care to include pollution control, occupational safety, ecosystem protection, and environmental justice.
In revealing how environments silently influence neurological survival, ALS research offers critical insight into the broader relationship between human health and the integrity of the environments we inhabit.










Comments
Post a Comment